- 8149143338
- Mon-Sat 8:00am to 11:00pm (By Appointment)
- nucleusivf@gmail.com
Natural Cycle IVF (also known as ‘Natural IVF’), is IVF which is carried out within a natural menstrual cycle without the use of fertility drugs. Natural IVF aims to collect just the one egg that has been naturally selected and matured by the body. This type of treatment is more affordable and safer than other forms of IVF. By utilising natural selection it is hoped that a high quality egg will be collected and therefore a high quality embryo created.
Growing success rates: We have pioneered a new approach with Natural Cycle IVF, where we combine a better understanding of ovarian physiology, our advances in ultrasound techniques and our medical and scientific expertise to deliver the optimum treatment.
Giving a chance to everyone: Many women are told that they cannot have a child with their own eggs because their AMH is too low, their FSH is too high, they have low ovarian reserve or that they are poor responders to fertility drugs. At CREATE, we are have an excellent track record in treating women in these circumstances with Natural IVF. We are able to tailor treatment with no or low amounts of stimulation drugs, thereby giving you the best chance to have a baby with your own eggs. We have successfully treated hundreds of women with critically low ovarian reserve/low AMH/high FSH. We have also had some of the oldest IVF mothers in the world who have had babies with their own eggs. We do not have any selection criteria and will allow any woman to try IVF using their own eggs if they want to and are still ovulating (up to the age of 50).
Higher quality egg and better implantation: The egg which is naturally selected by the body can be of higher quality than those produced in a stimulated IVF cycle. In addition, high stimulation drugs can adversely impact the environment of the womb and the lining of the womb. By avoiding stimulating drugs, the womb is more receptive to pregnancy. There is also evidence that babies born with Natural Cycle IVF are more likely to be born at full term and with a healthier birth weight.
A more natural and patient-friendly way of performing IVF: The Natural IVF cycle involves the collection of a naturally produced egg without medication, with the fertilised embryo being placed back into a drug-free womb. Natural IVF is therefore the closest that IVF treatment can get to natural fertilisation. Natural IVF Treatment is carried out in your natural menstrual cycle, unlike conventional IVF where your ovaries are first suppressed. The potential side effects and complications are therefore reduced in Natural IVF.
A safer option: The health and wellbeing of mother and child is our first priority. There is no risk of Ovarian Hyperstimulation Syndrome (OHSS) with Natural Cycle IVF. In addition, this in vitro fertilisation treatment offers a less invasive approach and the use of no/fewer drugs leads to fewer potential risks and side effects.
More affordable: Natural IVF is less expensive per cycle than Stimulated IVF treatments as it does not require a daily dose and cumulative dose of costly medications.
Can be repeated in consecutive cycles: Patients who choose this option can repeat their treatment in consecutive cycles – whereas, due to the effect of ovarian stimulation drugs on the body, Stimulated IVF patients need to take a two to three month break between cycles.
All women who ovulate can have Natural Cycle IVF. It is particularly suitable for older women, those with low ovarian reserve or those that are poor responders to fertility drugs. It gives the opportunity for some women to have a child with their own eggs, rather than donor eggs. It is also often chosen by those that want to avoid fertility drugs and associated risks and side-effects. Women who come to our clinics can choose to have Natural Cycle treatment as their first choice.
The first step is to come in for an initial scan and consultation. At this appointment the doctor will assess your situation and devise a personalised treatment plan. After this, you will come in 2 weeks before the start of your period to meet with a nurse. They will talk you through your treatment and go through the consent forms with you. You will then call up on the first day of your period (day 1) to book in your first scan. This will probably be on day 5, but could be earlier or later depending on the advice of the doctor. After the first scan, there will be around 2 or 3 more scans, usually performed every other day. The egg collection is generally performed on around day 12; this is carried out under sedation, and is followed by the embryo transfer a few days later.
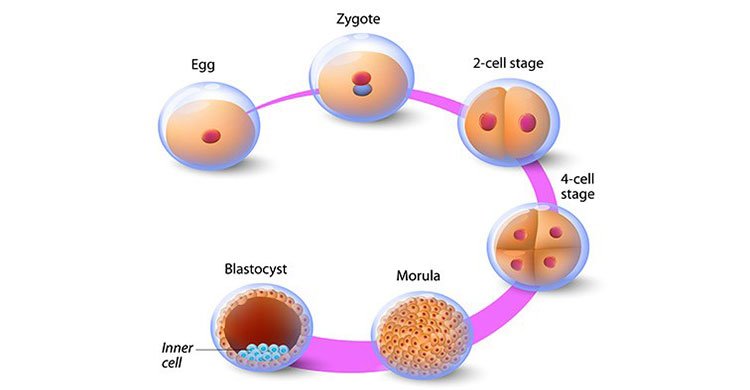
In vitro fertilization (IVF) involves several steps — ovulation induction, egg retrieval, sperm retrieval, fertilization and embryo transfer. One cycle of IVF can take about two weeks, and more than one cycle may be required.
Ovulation induction : If you’re using your own eggs during IVF, at the start of a cycle you’ll begin treatment with synthetic hormones to stimulate your ovaries to produce multiple eggs — rather than the single egg that normally develops each month. Multiple eggs are needed because some eggs won’t fertilize or develop normally after fertilization. You may need several different medications, such as:
Medications for ovarian stimulation : To stimulate your ovaries, you might receive an injectable medication containing a follicle-stimulating hormone (FSH), a luteinizing hormone (LH) or a combination of both. These medications stimulate more than one egg to develop at a time.
Medications for oocyte maturation : When the follicles are ready for egg retrieval — generally after eight to 14 days — you will take human chorionic gonadotropin (HCG) or other medications to help the eggs mature.
Medications to prevent premature ovulation : These medications prevent your body from releasing the developing eggs too soon.
Medications to prepare the lining of your uterus : :On the day of egg retrieval or at the time of embryo transfer, your doctor might recommend that you begin taking progesterone supplements to make the lining of your uterus more receptive to implantation. Your doctor will work with you to determine which medications to use and when to use them.
Typically, you’ll need one to two weeks of ovarian stimulation before your eggs are ready for retrieval. To determine when the eggs are ready for collection, your doctor will likely perform:
Typically, you’ll need one to two weeks of ovarian stimulation before your eggs are ready for retrieval. To determine when the eggs are ready for collection, your doctor will likely perform:
Vaginal ultrasound : An imaging exam of your ovaries to monitor the development of follicles — fluid-filled ovarian sacs where eggs mature.
Blood tests : To measure your response to ovarian stimulation medications — estrogen levels typically increase as follicles develop and progesterone levels remain low until after ovulation.
Sometimes IVF cycles need to be canceled before egg retrieval for one of these reasons:
Inadequate number of follicles developing.
Premature ovulation.
Too many follicles developing, creating a risk of ovarian hyperstimulation syndrome.
Other medical issues.
If your cycle is canceled, your doctor might recommend changing medications or their doses to promote a better response during future IVF cycles. Or you may be advised that you need an egg donor.
Egg retrieval can be done in your doctor’s office or a clinic 34 to 36 hours after the final injection and before ovulation.
During egg retrieval, you’ll be sedated and given pain medication.
Transvaginal ultrasound aspiration is the usual retrieval method. An ultrasound probe is inserted into your vagina to identify follicles. Then a thin needle is inserted into an ultrasound guide to go through the vagina and into the follicles to retrieve the eggs
If your ovaries aren’t accessible through transvaginal ultrasound, an abdominal surgery or laparoscopy — a procedure in which a tiny incision is made near your navel and a slender viewing instrument (laparoscope) is inserted — may be used to guide the needle.
The eggs are removed from the follicles through a needle connected to a suction device. Multiple eggs can be removed in about 20 minutes.
After egg retrieval, you may experience cramping and feelings of fullness or pressure.
Mature eggs are placed in a nutritive liquid (culture medium) and incubated. Eggs that appear healthy and mature will be mixed with sperm to attempt to create embryos. However, not all eggs may be successfully fertilized.
If you’re using your partner’s sperm, he’ll provide a semen sample at your doctor’s office or a clinic through masturbation the morning of egg retrieval. Other methods, such as testicular aspiration — the use of a needle or surgical procedure to extract sperm directly from the testicle — are sometimes required. Donor sperm also can be used. Sperm are separated from the semen fluid in the lab.
Fertilization : Fertilization can be attempted using two common methods:
Insemination :During insemination, healthy sperm and mature eggs are mixed and incubated overnight.
Intracytoplasmic sperm injection (ICSI) :In ICSI, a single healthy sperm is injected directly into each mature egg. ICSI is often used when semen quality or number is a problem or if fertilization attempts during prior IVF cycles failed.
In certain situations, your doctor may recommend other procedures before embryo transfer.
Assisted hatching :About five to six days after fertilization, an embryo “hatches” from its surrounding membrane (zona pellucida), allowing it to implant into the lining of the uterus. If you’re an older woman, or if you have had multiple failed IVF attempts, your doctor might recommend assisted hatching — a technique in which a hole is made in the zona pellucida just before transfer to help the embryo hatch and implant.
Preimplantation genetic testing :Embryos are allowed to develop in the incubator until they reach a stage where a small sample can be removed and tested for specific genetic diseases or the correct number of chromosomes, typically after five to six days of development. Embryos that don’t contain affected genes or chromosomes can be transferred to your uterus. While preimplantation genetic testing can reduce the likelihood that a parent will pass on a genetic problem, it can’t eliminate the risk. Prenatal testing may still be recommended.
Embryo transfer : Embryo transfer is done at your doctor’s office or a clinic and usually takes place two to six days after egg retrieval.
You might be given a mild sedative. The procedure is usually painless, although you might experience mild cramping.
The doctor or nurse will insert a long, thin, flexible tube called a catheter into your vagina, through your cervix and into your uterus.
A syringe containing one or more embryos suspended in a small amount of fluid is attached to the end of the catheter.
Using the syringe, the doctor or nurse places the embryo or embryos into your uterus.
If successful, an embryo will implant in the lining of your uterus about six to 10 days after egg retrieval.
After the embryo transfer, you can resume your normal daily activities. However, your ovaries may still be enlarged. Consider avoiding vigorous activity, which could cause discomfort.
Typical side effects include :
Passing a small amount of clear or bloody fluid shortly after the procedure — due to the swabbing of the cervix before the embryo transfer.
Breast tenderness due to high estrogen levels.
Mild bloating.
Mild cramping.
Constipation.
If you develop moderate or severe pain after the embryo transfer, contact your doctor. He or she will evaluate you for complications such as infection, twisting of an ovary (ovarian torsion) and severe ovarian hyperstimulation syndrome.


Nucleus IVF Centre has been providing quality IVF care with internationally comparable services and success rates. Our core strength lies in our ability to give to our patient’s comprehensive ART and allied services.
Copyright ©2022 NUCLEUS IVF. All Rights Reserved
Managed By Nucleus IVF